
Ebenezer Tumban (BioSci) was quoted in the story “MTU virologist discusses virus differences,” in the Daily Mining Gazette:
MTU virologist discusses virus differences
Joshua Vissers, Associate Editor, Daily Mining Gazette, March 27, 2020
HOUGHTON — Influenza and coronaviruses both travel between the infected wrapped in a stolen bit of the previous host cell’s outer, lipid-based layer called an envelope. That layer protects the viruses from harsh environments, and works as a kind of disguise to help them inject themselves into the next cell. The difference that makes an outbreak of coronavirus so much more dangerous is the difference in that envelope.
“Normally, envelope viruses are not stable in the environment,” Ebenezer Tumban said.
Tumban is a molecular virologist and vaccinologist at Michigan Technological University. He’s been studying viruses in an effort to learn how to vaccinate against them.
Envelopes dry out and deteriorate fairly quickly outside the body, and the virus inside is rendered helpless to infect another cell, he said.
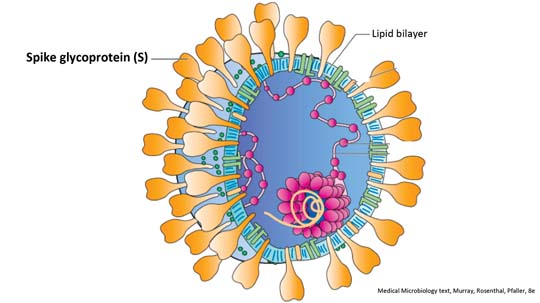
However, coronaviruses have hollow proteins embedded in their envelope. Scientists thought this structure looked like a crown, and so called it corona (Latin for crown).
“The crown basically makes them more stable compared to the regular flu,” Tumban said.
This extra stability allows it to last longer in the air and on surfaces compared to influenza viruses. So a coronavirus-infected person coughing in an area can infect people passing though that area for much longer than someone with influenza.
Despite having symptoms quite similar to a flu, fighting a coronavirus is more difficult for the body than fighting a flu virus for a few reasons.
“There’s a lot of things, some of it has to do with the virus and some of it has to do with us,” Tumban said.
A more stable envelope means the virus can exist in more parts of the human body. The flu virus is typically destroyed by fluid in the gastrointestinal tract, but COVID-19’s corona protects them from that, according to Tumban.
The virus also seems to be able to suppress immune system response in some people.
“People that were infected with coronavirus had a low level of lymphocytes,” he said.
This suggests that the coronavirus is also infecting those types of cells, which are part of the body’s defense system. The influenza virus doesn’t do that.
Tumban said there’s also evidence that the virus can trigger a reaction in the body similar to an allergic reaction.
“My body might overreact and produce a lot of cytokines,” he said.
These cytokines can trigger sepsis and organ failure in severe cases.
And medical professionals have fewer tools to fight coronavirus, too.
“We don’t have a vaccine for corona, we have a vaccine for influenza,” Tumban said.
Influenza vaccines have been in use for a long time, training our immune systems in how to make antibodies that fight that particular virus and creating a group immunity that protects even those without the vaccine. While the flu virus does mutate regularly, it’s rarely enough to render a vaccine entirely ineffective.
“Vaccinations from the past might help to make the disease less severe compared to coronavirus which is new,” Tumban said. “You don’t have a single antibody against it in your body.”
People hospitalized with the flu can receive certain treatments like Tamiflu, but Tumban said with coronavirus, doctors right now mostly give “supportive care” – using tools like ventilators to support the patient’s body while it fights or endures the infection on its own.
These factors together create a much more deadly virus than the flu.
“The mortality rate is about 10 times that of influenza,” Tumban said on Tuesday.
Tumban’s calculations, based on numbers from the Centers for Disease Control, show that a high estimate of influenza’s mortality this year is about 0.1% in the United States, but coronavirus is showing to be about 1.27%.
Worldwide, the mortality rate for coronavirus is about 4.3% according to Tumban.
The increased mortality and lack of treatment and defense are what is leading countries and organizations around the world to implement social distancing and quarantine measures as healthcare providers ramp up capacity and researches search for vaccines.
However, while coronavirus can be far more infectious and harmful than the influenza virus, many of the same precautions work to prevent infection. The No. 1 recommendation, hand washing and sanitizing, destroys the all-important envelope protecting the virus, rendering it virtually harmless.
“There’s no way they can cause the disease,” Tumban said.
Editor’s Note: This story has been changed to more accurately portray Dr. Tumban’s work. While he has worked directly with Zika, dengue, HPV and other viruses, he has not worked directly with coronaviruses.