Presenters, organizers, and some attendees of the second MTU / MSU collaborative research symposium pose for a group photo.
Developing novel approaches to fighting disease, using machine learning and computational methods to solve epidemiological problems and improve patient health, and applying technologies to intervene on disease. These are just a few of the challenges and ambitious solutions facing the state of biomedicine now and in the future. These topics, and several others, were addressed at a recent invitation-only collaborative research symposium between MTU and MSU.
On Friday, Oct. 27, 2023, groups of researchers from Michigan Technological University and Michigan State University University met in a collaborative research symposium.
Entitled Engineering the Future of Human Health II: Biomedicine in the 4th Industrial Revolution, this event was held in Michigan Tech’s Memorial Union Building.

The symposium preceded the Upper Peninsula Medical Conference, put on by MTU’s Health Research Institute, which focused on diverse approaches to health challenges affecting rural communities. It marked the second collaborative research symposium between these two universities. That is, Michigan State University College of Human Medicine hosted the first symposium on March 13, 2023. It was held in MSU’s beautiful Secchia Center in Grand Rapids, Michigan.
Delivering Short Talks With A Big Impact
For these symposiums, the goals continue to be learning about each other’s work; and investigating areas of shared objectives, mutual interests, and possible research projects between MTU and MSU. But perhaps the even greater purpose is that of these institutions combining forces (and resources) to tackle the most challenging health-related issues of the upcoming decades.

To disseminate as much research as possible, presenters kept their talks brief. In total, 12 researchers from MTU and 11 from MSU delivered rapid-fire, ten-minute presentations in six consequent sessions exploring the state of biomedicine in the era of Industry 4.0:
- Computational Health Science (Session 1)
- Big Data in Healthcare (Session 2)
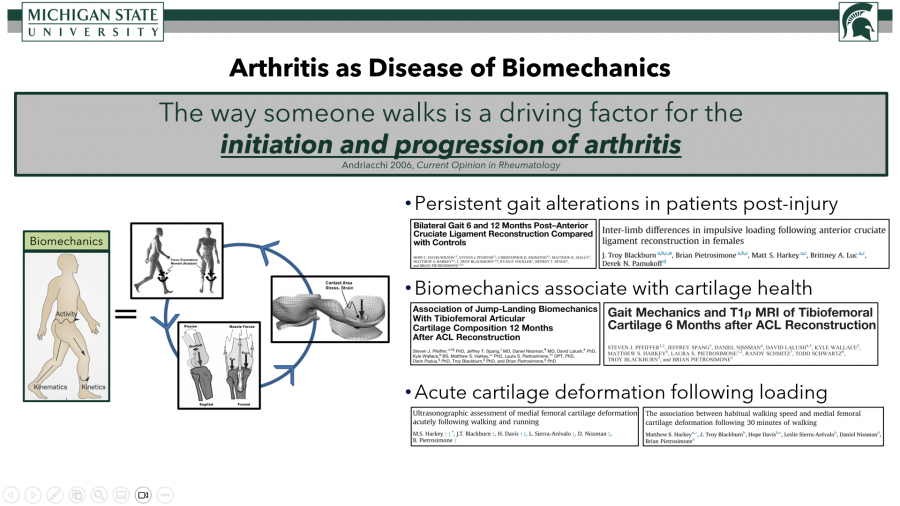
- Kinesiology and Physiology (Session 3)
- Neural Control and Disease (Session 4)
- Metabolic Disease (Session 5)
- Chemical Biology (Session 6)
This structure provided opportunities for researchers not only to learn from each other, but also to explore possible connections between their fields.
And the fields were, indeed, diverse. That is, professionals at this multi-disciplinary event came from applied computing, biological sciences, biomedical engineering, chemical engineering, chemistry, computer science and engineering, kinesiology and integrated physiology, pediatrics and human development, and quantitative health sciences. Overall, the quality of the research and breadth of disciplines spoke to the depth of expertise at this symposium and to the challenges and opportunities facing the future of biomedicine.
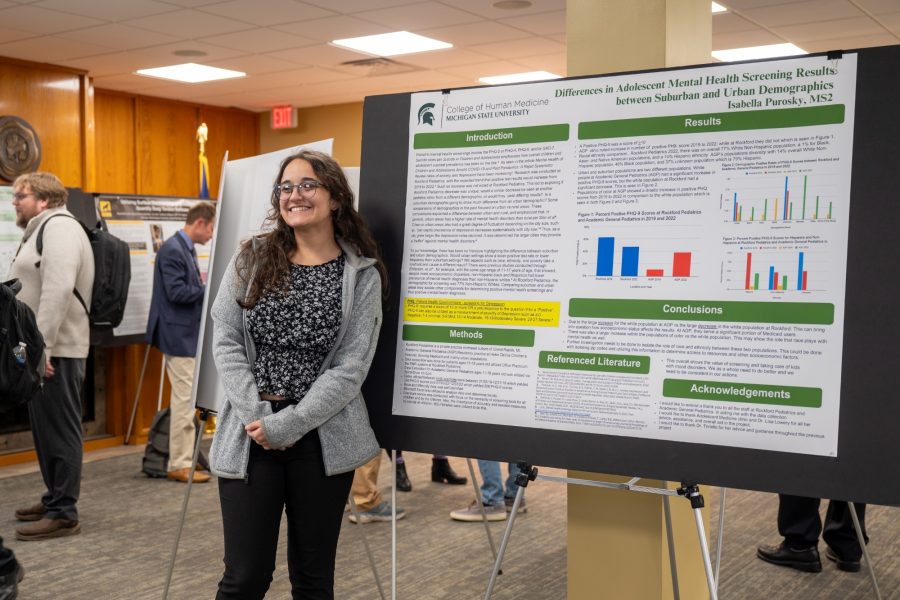
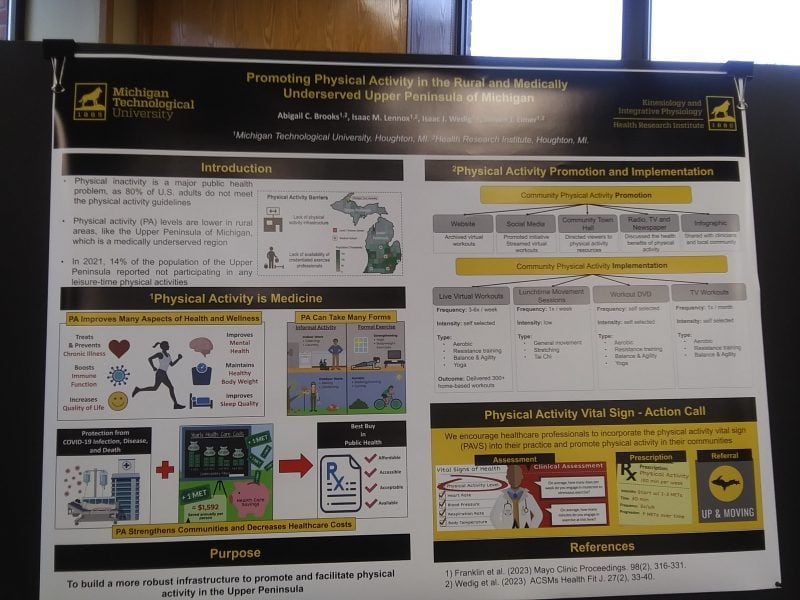
There was also a concurrent combined poster session with the UPMC that featured research from several MSU and MTU students, as well as a few professors.
Exploring Connections Between MTU and MSU
Throughout the symposium, there were several salient connections both within and between sessions. For instance, many experts presented on novel treatments for conditions and/or diseases affecting public health, such as diabetes, cancer, cystic fibrosis, neurodegenerative disorders, and lack of activity. Dr. Ping “Peter” Wang (MSU, Session) tackled integrating bioengineering into Type-1 Diabetes treatment. And Dr. Marina Tanasova (Session 6, MTU), after summarizing the role of GLUTs (Glucose transporters) in various diseases, focused on targeting these GLUTs in cancer therapy. Dr. Ashutosh Tiwari (Session 4, MTU), analyzed the role of protein aggregates (misfolded proteins) in the cellular toxicity central to neurodegenerative diseases.
Another common thread was responding to the continuing public health crisis of Covid-19. For example, the symposium began with the long research project of Dr. Jeremy Prokop (MSU, Corewell Health) on genotyping various Covid variants. Then, he shifted to how the immunosuppression connected to Covid-19 is associated with the emergence of other viruses, such as Epstein-Barr (EB) and the Human Papillomavirus (HPV).
Throughout the symposium, several experts also assessed the leveraging of artificial intelligence and computational approaches to address health ailments. Dr. Hoda Hatoum (MTU, Session 1) presented on experimental and computational approaches to model cardiovascular diseases and therapies.
There were also presentations on more low-tech, but nonetheless impressive, methods for improving patient outcomes. Dr. William Cooke (MTU, Session 3) demonstrated how using a rather simple impedance-threshold breathing device can reduce hemorrhaging. Using Blood Flow Restriction (BFR) to increase exercise intensity without taxing joints (MTU, Session 3) was the topic of Dr. Steve Elmer’s presentation.
Targeting the Youth Mental Health Crisis in Michigan
CHI Program Director Dr. Guy Hembroff spoke on using AI to improve the mental health of youth (MTU, Session 2). He began by stressing some startling statistics from Youthgov on suicide in the 15-24 age group. Most striking was the fact that “taking one’s life is the second leading cause of death for youths.”

Hembroff proposed a number of strategies for using artificial intelligence to track, intervene on, and improve the mental health of youth.
First, he articulated that AI may be employed to not only enhance preventative mental health measures, but also provide safe, responsive data.
Or to put it another way, through wearables, daily mental health check-ins, and user feedback, youth could have personalized, responsive mental health treatment delivered right to them. In short, Hembroff outlined a protocol for providing inexpensive, effective tools that quickly monitor and respond to at-crisis youth, reduce the need for reactionary care, and prevent mental disease from spiraling into suicide.
There is another positive effect of this AI-assisted mental health plan: gamifying the activity of tracking one’s mental health. Youth are known for always interacting with their phones. Thus, this gamification could help reduce the stigma associated with reporting depression, anxiety, and other mental diseases.
Symposium Goals: Promoting Networking and Sharing Research
Hembroff’s talk captured one of the main threads of the symposium: using ingenious, cost-effective, computational approaches to solve crucial health issues. However, all of the research was impressive. That is, there were several expert scientific communicators, such as Zhiying “Jenny” Shan (MTU, Session 5), who walked the audience through her research on extracellular vesicles and blood pressure regulation.
But you can learn more about the depth and breadth of the research by examining the event schedule.
In the closing remarks for the symposium, Dr. Christopher Contag (MSU) further elaborated on the connections between these presentations and the opportunities for collaborative research. First, he summarized some commonalities, such as further analyzing cardiovascular disease, studying extracellular vesicles as diagnostic markers, developing strategies for early intervention, and creating a Long Covid research center.
In addition, Dr. Contag focused on the importance of learning the language of cells and communicating with them: that is, this research is about “not just asking them what they’re saying, but telling them what to do.” He saw this communication as central to modulating the immune system and to controlling disease states.

“I think we’re all focused on distributed healthcare and using our approaches and innovation to reduce health disparities. It’s a theme that’s shared between the two universities.”
Moving Beyond This Symposium
For Engineering the Future of Human Health II, MTU’s cosponsors were David Lawrence, vice president for Global Campus and continuing education; Dr. Sean J. Kirkpatrick, professor and department chair, Biomedical Engineering; Dr. Caryn Heldt, professor in Chemical Engineering and director of the Health Research Institute; and Dr. William H. Cooke, professor and department chair, Kinesiology and Integrative Physiology. And for MSU, Dr. Adam Alessio, Departments of Computational Mathematics, Science, and Engineering, Biomedical Engineering and Radiology; and Dr. Bin Chen, associate professor, Department of Pediatrics and Human Development took on the roles of cosponsors.
This collaborative symposium is crucial to the MTU Global Campus mission of helping Michigan Technological University grow partnerships with other higher-ed institutions and participate in multidisciplinary research that tackles pressing biomedical challenges.
The next step, then, is instituting these collaborative working research groups. Furthermore, the two universities hope to pool both talent and resources to build a MSU / MTU translational research center in Grand Rapids, MI. Of this center, David Lawrence further articulated its two main objectives: “first, developing cutting-edge health technologies through advanced applied biomedical research; and, second, but equally important, ultimately improving the health of the citizens of Michigan and those of the nation.”
Readers can also learn more about this event in the coverage by TV6.